Amelia’s Birth Story Part 2: C-Section & Umbilical Cord Prolapse
Part 1 can be found here.
(Content warning: umbilical cord prolapse, birth trauma, emergency cesarean, NICU stay.)
I verbally consented to the emergency c-section. The nurses in the room flew into action, breaking down the bed and lifting my hips up into the air. One nurse had to place her hand inside me on the baby’s head to keep it from putting too much pressure on the cord. I asked a few questions and was quickly wheeled to the OR.
If you’ve ever watched medical shows (think Grey’s Anatomy) or seen a movie in which a trauma happens, sometimes there’s a scene from the patient’s point of view of being rushed to the OR. They look up at the ceiling and count the bright overhead lights as they pass by. That’s how I felt as I was rushed to the operating room - like I was in an episode of Grey’s Anatomy, only it was real life and way more terrifying. I was shaking as I was wheeled to the room, surrounded by so many people, and they tried to cover me the best they could but that was difficult with a nurse’s hand basically inside of my uterus. Meanwhile, Jeremy was left alone in the first delivery room. I told him to call our families, but it was in the middle of the night at that point and everyone was asleep.
They moved me to the operating table and started to prep my body for surgery. They started cleaning my belly and I called out “Wait, am I going to be asleep for this?!” They assured me that I would and that everything would be okay. A very nice nurse with glasses grabbed my left hand and helped calm me down. I was trying not to cry, but whatever she said made me feel less alone and less scared. I saw my doctor come into the room, fully scrubbed in. The anesthesiologist started talking to me calmly, and I just remember looking up into his blue eyes as he put an oxygen mask on my face. I told myself that I should just close my eyes and count down in my head, and when I wake up my baby will be here.
I was right. I woke up to the sound of my baby crying. Nurses were moving all around me. My stomach hurt so bad, my throat hurt, I was hungry, and I was loopy on the IV pain meds they gave me. Jeremy came over to me holding Amelia and the nurses asked if I wanted to hold her. I said no, because I was worried I would drop her. Then I swear she cried “mama,” and I yelled for Jeremy to give her to me. It could have been the pain meds, but I know the nurses in the room heard it too!
I held her for a few minutes before she was taken to be examined. Her oxygen was low, as expected from the pressure on her umbilical cord, so they wanted to take her to the NICU to be monitored. My doctor came into the room to check on me, and I don’t remember what she told me, but in my loopy state I asked her, with tears in my eyes, if Amelia was the most beautiful baby she had ever seen. Then I announced to her, and anyone else who would listen, that my husband would be getting a vasectomy after this ordeal. It was kind of hilarious, and despite the trauma, I still had my sense of humor. Or I was just loopy from the pain meds. I also kept asking all of the nurses for food, stronger pain meds, and then I tried to take a nap.
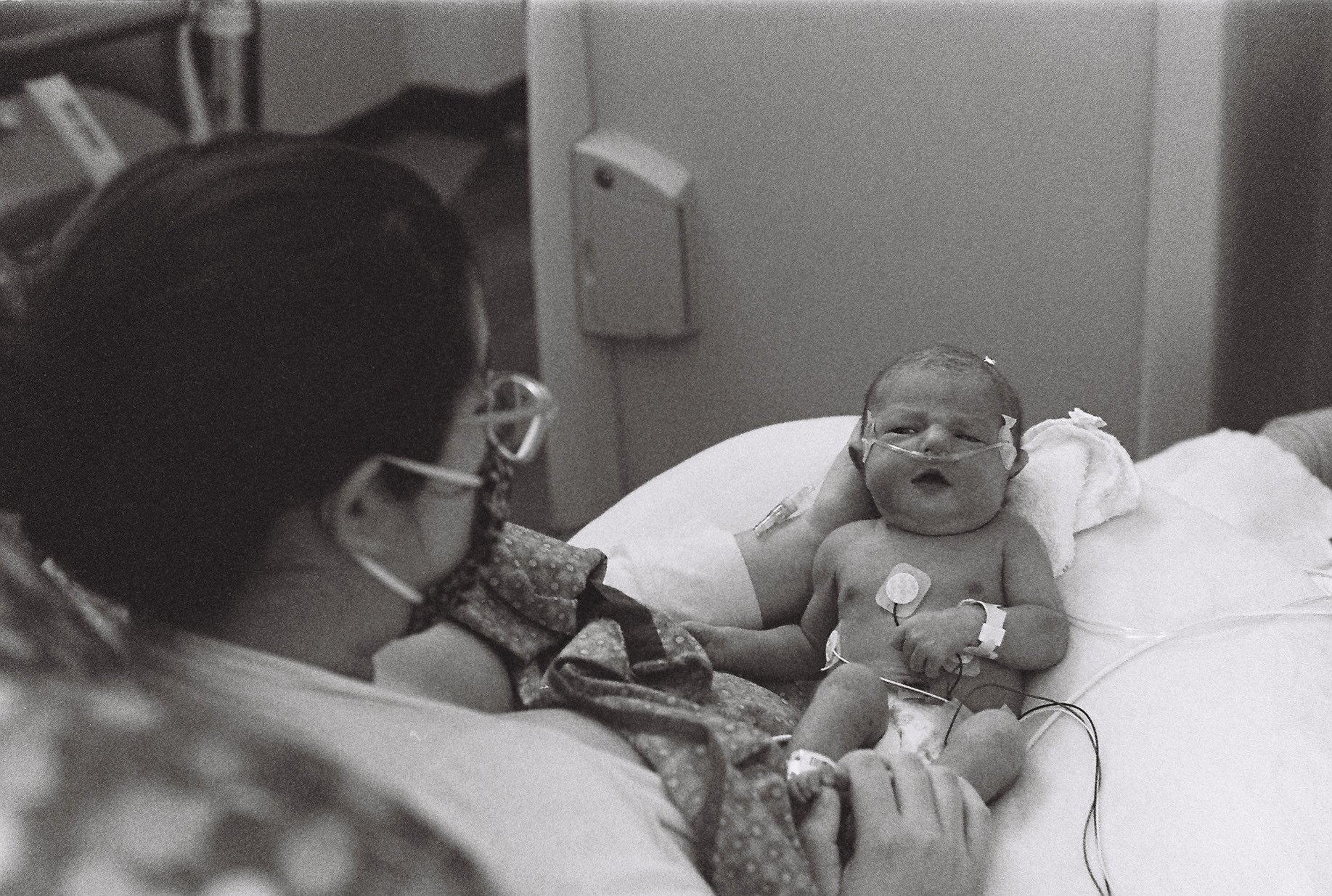
It was a while before I was able to go see my baby in the NICU. I was exhausted and in a lot of pain. I was afraid to walk or move around too much. I pumped milk for her as soon as could, but I mostly focused on resting and feeling better. I had to have an iron infusion because my iron was so low at the end of my pregnancy. I don’t know exactly when, but 12-24 hours after she was born, I made my way over to see my baby. I was so nervous to hold her with all of the cords and monitors. I began nursing her and she latched right away.
Our hospital stay was lonely. Jeremy stayed with Amelia in the NICU and would come visit me and bring me to her when I was up for it. He would help me shower and make sure I ate, but neither of us wanted Amelia to be alone for very long. Since I couldn’t have any visitors (COVID-19 protocols), I was alone in my room for most of the time. I cried a lot, especially the first day. I also slept a lot, which I think helped my recovery. I spent as much time in the NICU as I could, but sitting up in a chair or standing for too long took a lot out of me.
We facetimed our families and our older daughters as much as we could. Although my girls couldn’t be there to meet their baby sister yet, my oldest got to watch Amelia have her first bath over facetime. Our stay was only about 4 days, but it felt longer. Luckily, Amelia was able to be discharged from the NICU after I was discharged from the maternity ward. She didn’t need to stay on oxygen for her entire NICU stay, but she had swallowed a lot of blood during her birth which concerned the pediatricians. Regardless, she was thriving when it was time to go home.
It took months for me to process the trauma from my daughter’s birth. I still cry when I think about it sometimes, even as I was typing this post. My baby is a happy, healthy, 17 month old toddler, but it feels like her birth happened yesterday. Jeremy and I spent countless nights during her first year talking about what happened. We both have felt anger and grief, and then guilt because we know how lucky we are that our baby was okay. I blamed myself for what happened - maybe things would have been different if I had labored at home longer, or if I had put my birth preferences in writing. Then I remember the awful feeling in my gut that day and I wonder: If my water broke on its own at home like it did with my first two, would I be telling a much sadder story?
I’ve spent so much time wondering the “what-ifs,” but I am here now with the “I knows.” I know that we could not have anticipated umbilical cord prolapse. I know that an emergency c-section brought my baby into the world alive. I know that it caused me trauma. I know that I am healing from that trauma a little more each day. I am grateful for my daughter’s health and safety, and ultimately for her life. It was not the birth I wanted to have, and it’s okay for me to mourn that, especially since she’s my last baby. It’s also okay for me to celebrate the fact that an emergency cesarean saved my baby’s life. I don’t have to choose between happy or sad - that’s often the case with birth trauma. It is a mix of complicated feelings, and one feeling does not invalidate another.
It’s heavy, but I don’t mind sharing my experience. Thank you for reading our story.